Note: The author acknowledges Arun Jatkar, Monroeville, PA; Lalit Mohan Gantayet, Navi Mumbai, India; Verghese Chandy, Melbourne, Australia; and K. Suryanarayanan, Chennai, India for their thoughtful review and suggestions on the drafts before it was finalized.
By now everyone has seen them — horrifying images of mass cremations on open grounds in newspapers, and flashed on TV screens across the globe. Gory video clips showed in blatant invasion of privacy, decency, and sensitivity, patients in trauma minutes away from death in crowded New Delhi’s ICUs. They dared not show these scenes that routinely did happen in ICUs across the US a scant ten months earlier. Denigrating India is fair game in the global media.
In April-May the second wave of the pandemic hit the Indian middle and affluent classes as well. The widely reported shortage of medical oxygen, a routine item in normal times, for Covid patients in ICUs only accentuated the issue. The polyglot voices of politicians and opinion writers in the ratings-driven Indian media understandably pinned down Prime Minister Modi, berating him for everything that went wrong.
What the Indian media, or international media, did not highlight is the lackadaisical response of state governments and the profiteering attitude of the profit-driven private hospitals that led to the oxygen shortage. Here (www.tinyurl.com/GurumurthyO2) is a story on how the shortage was precipitated by profit-driven private hospitals.
Here (www.tinyurl.com/GulfNewsOnModi) is another story discussing whether the Modi government was negligent. The drift of this article is that a) the Modi government did anticipate the second wave, and did warn state governments; b) opposition parties did not want the Modi government to ban open election rallies during the pandemic; and c) the Modi government expanded the medical infrastructure (isolation beds and ICUs) by several multiples during the pandemic. Granted, whatever was done was not adequate given the enormity of the pandemic.
India’s pandemic crisis needs to be seen in the global context. See the table below.
Mortality Table for Select Countries (data from WHO)
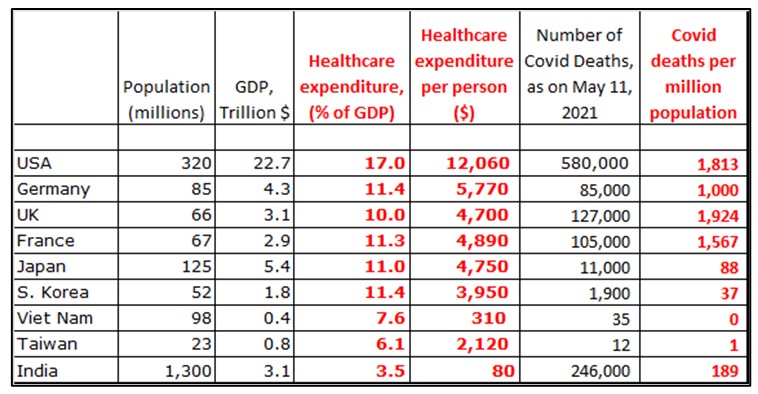
• The US and the industrialized West, despite its high GDPs (column 3), high expenditure on healthcare as a % of its GDP (column 4), high per-capita healthcare expenditure (column 5), high standards of living, and far better healthcare infrastructure than the rest of the world, did poorly in managing the Covid pandemic (last column).
• Taiwan, South Korea, Japan and Vietnam, neighboring China from where the Covid pandemic originated, responded much better than the industrialized West. Compare the numbers in the last column. Vietnam is a developing economy. What did they do right that the West did not, and did we learn anything at all from them?
• In India, the officially reported mortality rate is ~200/million, even with its poor investments in healthcare (more on this later). It is quite possible that India under-reported or misclassified its mortality numbers. Even if we assume India’s actual mortality rate is twice, or thrice (that is, 100% or 200% more), it would still be ~400/million or ~600/million, not anywhere near the more than 1,800 deaths/million in the US.
• But with India’s free, confrontational media hostile to Modi, and with NGOs everywhere, deliberate large-scale suppression of Covid mortality data is not easy in India’s federal system of governance. All Covid-positive diagnoses and deaths nation-wide have to be immediately reported to the Indian Council of Medical Research that gathers and collates all raw data and keeps a close watch on this pandemic’s spread.
India’s Healthcare System:
In the Indian constitution, healthcare is a state subject with democratically elected governments driving the healthcare policies in each state. This is because of India’s demographic diversities in every metric and wide variations in available resources and priorities. With disparate political parties at loggerheads with each other running the 30-plus state governments, massive, deliberate fudging of covid mortality numbers would be difficult for the federal government.
The profit-driven Indian healthcare industry is unregulated, modeled after the American pay-per-service system (but without any oversight). Private general practitioners are at the bottom of the pyramid with specialists in the expensive super-specialty hospitals at the top.
The poor/working poor go to the inadequately funded, poorly equipped, and badly managed government hospitals for all their needs; in these hospitals, the service is free, but far from satisfactory. Government hospitals train new doctors with dedicated senior clinicians drawn by the challenges to serve the poor.
The poor cannot afford expensive pay-per-service private doctors. Consider this: tertiary medical care for a knee replacement + 2-week hospital stay costs INR 500,000 to 700,000 in a second-tier private hospital, way beyond the reach of working-class Indians earning and spending in rupees. The middle class go to private doctors and private hospitals they can afford. The rich go to the expensive super-specialty hospitals.
The Covid pandemic brought out many depressing features that have been festering for nearly six decades in India’s healthcare sector, with both omissions and commissions by different segments:
• Poor investment decisions in public health and primary care by state governments for over 70 years (Modi came to power only six years before the pandemic exploded).
• Unregulated pharmaceutical and medical supplies industry — many of them multinational companies based in the EU and the US.
• Practicing physicians owning medical labs with vested interests.
• The high cost of medical education in profit-driven private medical colleges run by politicians under the rubric of tax-exempt foundations. The cost of fees plus books and supplies in a profit-driven private medial college for a five year program exceeds INR 10,000,000 (or 1 crore rupees). To this you need to add the cost of boarding and lodging. Freshly minted doctors coming our of medical colleges with this kind of “investment” are in a great pressure to recover the money as quickly as possible.
• Low tax base for the governments (more on this later); and
• The sinister practice of unethical, illegal payments permeating the entire healthcare industry.
The last item is pernicious and needs some elaboration:
• All drug companies — European, American and Indian — bribe doctors in India for prescribing their medications on a prorated basis. The more you prescribe, the more you get as bribe.
• Specialists bribe general physicians to refer patients to them.
• Labs bribe physicians and surgeons to refer patients to their labs for blood work, pathological tests, and X-rays, CT-scans, etc.
• Hospitals bribe doctors for referring patients into their facilities.
• Often the doctors themselves own these labs, tempting them to order more tests than what are needed.
All these unethical and illegal payments are deviously transferred to patients, who often do not have health insurance and bear 100% of the cost from their own pockets. These payments can be up to 40% of the final costs. The unscrupulous ways in which India’s healthcare industry — doctors, European, America, and Indian pharmaceutical companies, hospitals and medical labs — bilks helpless patients in India are well-known.
So, the industry of healthcare delivery is predatory and exploitative throughout India. Often, the interactions are hostile between private doctors and patients (who bare 100% of the cost of the medical care out of their own pockets). This is because of the lack of trust between the doctors and the patients when it comes to the need for tests, and how much they will be charged.
Thus, the impenetrable thicket of India’s healthcare industry is sustained by a mutually exploitative dependence among all segments of the unregulated healthcare system with no oversight. This system has been ripping off the hapless patients for over 50 years. No wonder there is no incentive for preventive and primary care in Indian healthcare system. END
